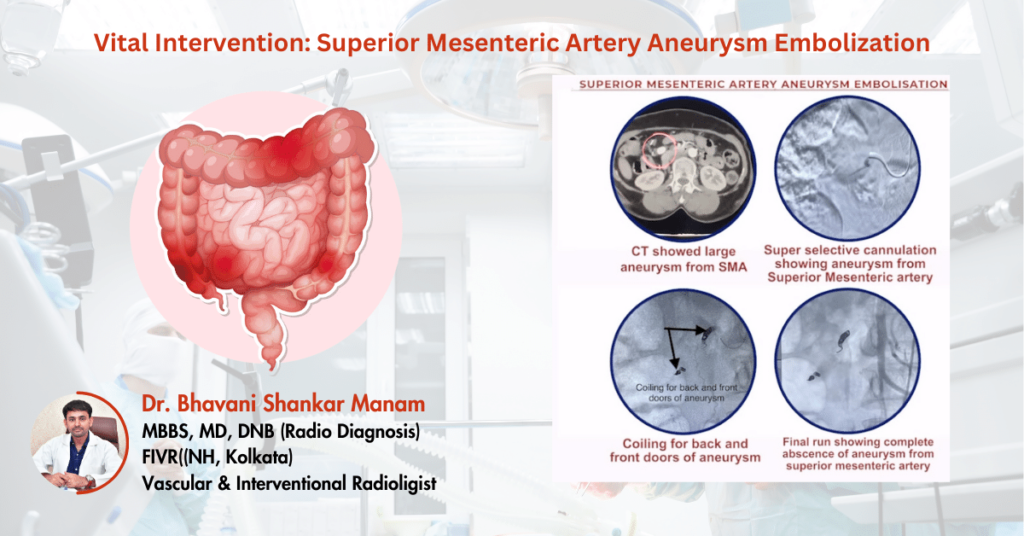
uccessful Embolization Procedure for Pulmonary Artery Pseudoaneurysm in a Tuberculosis Patient
This case study highlights the successful intervention in a 73-year-old woman who presented with life-threatening episodes of massive hemoptysis. Her medical history included a diagnosis of tuberculosis, which led to the formation of a large pseudoaneurysm in the left lower lobe segmental pulmonary artery. The medical team opted for an embolization procedure, which resulted in a positive outcome: no further hemoptysis episodes and a safe discharge.
Patient Presentation and Background
A 73-year-old woman arrived at the hospital experiencing sudden, severe hemoptysis—coughing up large amounts of blood. She had a known history of tuberculosis, a lung infection that often leads to complications such as pulmonary artery damage. Imaging studies revealed a large pseudoaneurysm in the left lower lobe segmental pulmonary artery, which was the source of the bleeding.
Diagnosis and Treatment Planning
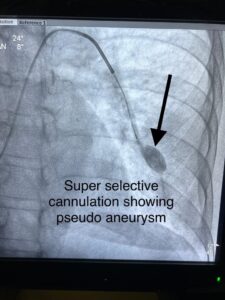
After a comprehensive evaluation, medical imaging confirmed the presence of the pseudoaneurysm. A pseudoaneurysm occurs when the wall of a blood vessel weakens and bulges, creating a blood-filled pocket that can rupture, leading to significant bleeding. To prevent the risk of rupture and further bleeding, the medical team decided on a minimally invasive embolization procedure to block the blood flow to the pseudoaneurysm.
Embolization Procedure: Minimally Invasive Approach
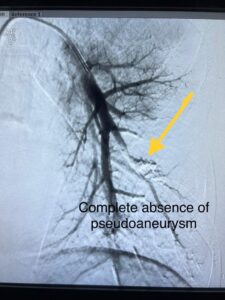
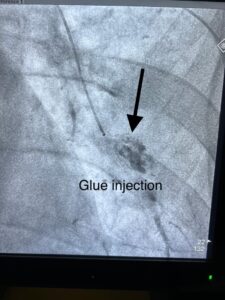
The embolization procedure involved a catheter inserted into a peripheral blood vessel, typically from the groin. Under fluoroscopic imaging, the catheter was guided to the site of the pseudoaneurysm. The medical team then deployed small coils or particles to block the blood flow into the aneurysm, effectively causing it to clot and preventing further bleeding.
Post-Procedure Outcome and Recovery
The embolization procedure was highly successful. The patient experienced no further episodes of hemoptysis, and imaging confirmed that the pseudoaneurysm had been effectively treated. The patient’s recovery was smooth, with no complications, and her condition improved significantly after the procedure.
Discharge and Follow-Up:
After careful monitoring and evaluation of the patient’s post-procedure progress, the medical team deemed her fit for discharge. She was given proper instructions for home care and advised to attend regular follow-up visits to ensure her continued well-being.
Conclusion:
In conclusion, this case study illustrates the successful management of a life-threatening pseudoaneurysm in a 73-year-old female with a history of tuberculosis-induced massive hemoptysis. The embolization procedure effectively addressed the condition, preventing further episodes of hemoptysis and facilitating the patient’s safe discharge. Early diagnosis, prompt intervention, and appropriate follow-up care were crucial in achieving this positive outcome. This case emphasizes the significance of timely and targeted interventions in managing complex medical conditions effectively.